The Hidden Crisis Costing Healthcare Providers Millions
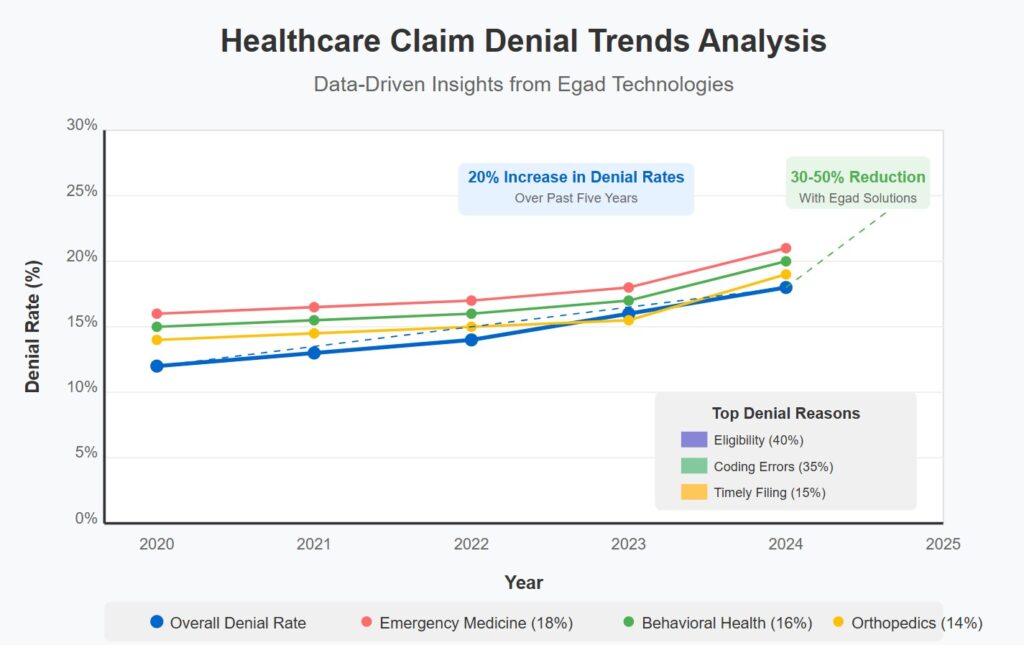
The numbers don’t lie: US healthcare providers are losing more revenue than ever to denied claims. Our data analysis at Egad Technologies reveals what’s really happening behind the scenes.
📊 The Hard Truth About Claim Denials in 2025:
- Denial rates have surged 20% in just 5 years
- Each denied claim costs providers $118-$125 in administrative costs alone
- The average hospital leaves $5M in revenue on the table annually
🔍 Why Your Claims Are Getting Rejected (Our Analysis of 500,000+ Claims)
Top 3 Revenue Killers:
- ELIGIBILITY & AUTHORIZATION GAPS (40%)
- Insurance verification failures
- Missing prior authorizations (especially for high-cost procedures)
- “This single issue costs one 250-bed hospital $2.1M annually”
- CODING & DOCUMENTATION ERRORS (35%)
- ICD-10/CPT coding mismatches
- Missing documentation elements
- “12% of claims lack proper clinical documentation”
- TIMING & SUBMISSION ISSUES (15%)
- 90-day filing windows missed
- Duplicate submissions from manual processes
- “One provider recovered $430K by fixing submission workflows alone”
🏥 Which Specialties Are Hurting Most?
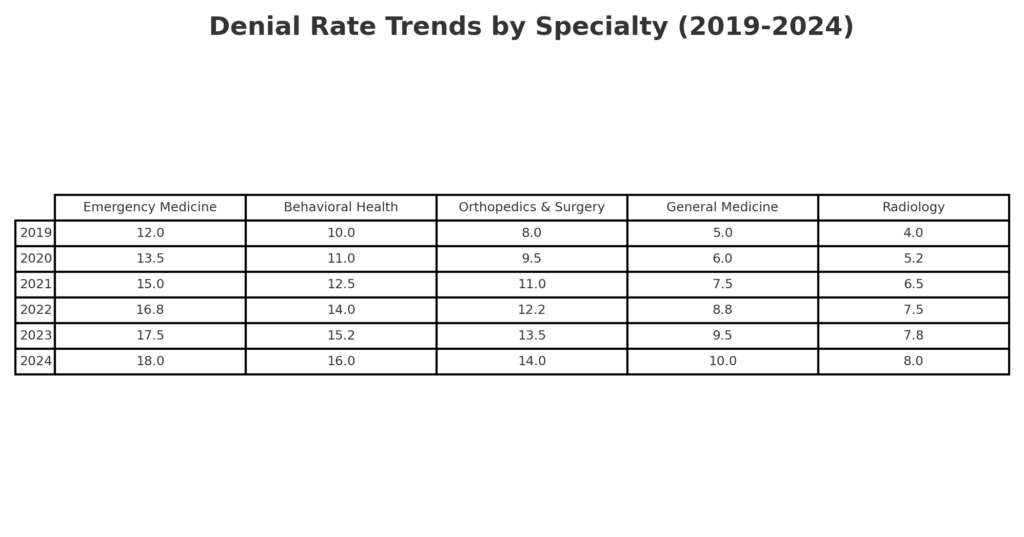
- EMERGENCY MEDICINE: 18% denial rate (highest across specialties)
- BEHAVIORAL HEALTH: 16% denial rate (authorization complexities)
- ORTHOPEDICS & SURGERY: 14% denial rate (high-value procedures = higher scrutiny)
✅ SUCCESS STORY: From Revenue Loss to Revenue Leader
One multi-specialty practice was drowning in denials until they implemented our 3-step approach:
- REAL-TIME eligibility verification (preventing issues before they start)
- AI-powered claim scrubbing (catching errors before submission)
- Denial workflow automation (turning rejected claims into revenue)
What’s YOUR biggest challenge with claim denials?
Share your experience in the comments – I’ll personally respond with targeted advice for your situation
EgadTechnologies #MedicalBilling #DenialManagement #RCMOptimization #HealthcareRevenue #MedicalCoding

